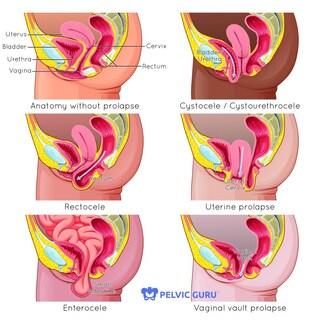
 By Rachel Miller, PT, DPT Prolapse is when one or more of the pelvic organs (bladder, uterus, rectum, intestines) move downward. Severe prolapse is when these organs come out externally, where a bulge can be seen or felt. Mild or moderate prolapse is more common. Symptomatically, prolapse can feel like pressure, heaviness or aching in the pelvic floor, or the feeling of a tampon falling out. Prevalence of prolapse has been difficult to confirm, especially given the fact that only 4-10% of women who have prolapse report symptoms. One research study discovered prolapse in 32% of women and a different study found prolapse in 98%, and other studies have shown numbers in between. While we are not sure exactly how many women it affects, it is a large percentage of middle-aged and older women. Risk factors for prolapse include increasing age, obesity, chronic constipation, vaginal delivery especially with trauma or episiotomy, smoking and giving birth to large babies. Women who have had a c-section are less likely to develop cystocele and rectocele but still are likely to develop uterine prolapse. Terms such as cystocele refer to which organ is prolapsed, in this case the bladder (see the picture for more details). There are different types of prolapse and you can have more than one at the same time. Prolapse is diagnosed with a pelvic exam (so ask your healthcare provider about it when you go next time) so you can know your body. The word prolapse can sound scary. And the statistics make you realize how many of us likely have some degree of mild prolapse without any symptoms. Don’t be afraid. I like to think of it as the organs have shifted during pregnancy, they were stretched and pushed down by baby. After delivery, our body is healing and reorganizing for up to a year postpartum. If you have prolapse right after having a baby, know that it will likely improve as you heal. If you have never had a baby or had a baby a long time ago, there is still hope. This is a wake up call to be proactive. We have control over our pelvic floor strength, and how we use our body all day long. What contributes to prolapse? Excess pressure, specifically downward pressure on the pelvic floor. Things like straining to have a bowel movement, pushing a baby out for hours. But also bearing down on your pelvic floor when you are doing strenuous activities such as lifting your kids, working out, even yelling. It is my belief that years of this excess pressure in combination with gravity and more hormone changes during peri-menopause may contribute to pelvic floor issues (such as prolapse and incontinence) later in life. While there are no studies to prove or disprove this, I believe that it is worth taking the time to work on your core and pelvic floor to help now and hopefully in the future. To be proactive, it is important to learn intra-abdominal pressure management strategies. Big words, right? What that means is learning how to use the inner core system functionally. The pelvic floor, abdominal wall, diaphragm, and deep back muscles all working together without putting excessive pressure on the abdominal wall or pelvic floor. A functional core system will not only help prolapse, but can also help with back pain and other issues as well. Unfortunately, it is not as easy as just doing one or two exercises. It is truly understanding where these deep muscles are and how to apply these concepts into your daily activities as well as other types of exercise. The goal is a functional, reflexive core system that provides support and stability. Whether you have prolapse or not, whether you have symptoms or not, right now is the best time to start. Permission to use copyright images from Pelvic Guru LLC.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
Get your free guideJust click on the picture: 7 Tips to help your back pain feel better without pain medication, injections, or surgery or Post-baby Body Basics: what every Woman needs to know about their postpartum body. CategoriesArchives
September 2022
|
|
1113 S. Milwaukee Ave
Suite 203 Libertyville, IL 60048 |
Copyright ©2020. The Pilates PT LLC. All rights reserved

 RSS Feed
RSS Feed
