|
by Rachel Miller, PT, DPT
Self Care. What does that phrase mean to you? There is not one right answer. I believe self care is what helps “fill your cup”, something that you are doing for yourself. Something that you do not NEED to do, but that you want to do. Self care is important for both your physical and mental health- though some activities can help both. Life for many of us is busy, even hectic at times. When our world was on pandemic pause in 2020, it was a reset. Many people had a chance to re-evaluate what was important to them and what relationships and activities they wanted to continue, and what to release. As we re-entered the world, we could choose which activities to return to, and think about how busy we wanted to be. For some of you, life probably looks similar to how it did before. For many of you, it doesn’t. And it is easy to be swept up into the hustle and bustle so do not forget to recharge. When my son was a newborn, my self care was taking a shower without worrying about a crying baby at any moment, going to the store by myself, or going to a workout class. Yes, I know most of us need to shower and go to the store- but often that was showering with a crying baby in the bouncer and going to the store without lugging the car seat in and out. Now that my kids are a little bit older, my self care has changed. It is working out. It is getting a pedicure once in a while. It is making sure to schedule a girls night out. A date night. For you, that may look different. Self care is about prioritizing YOU and doing things that bring you joy. A few other ideas to help get your mind thinking in the right direction…
0 Comments
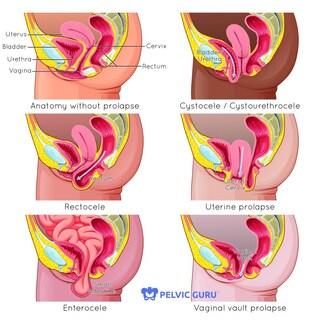 By Rachel Miller, PT, DPT Prolapse is when one or more of the pelvic organs (bladder, uterus, rectum, intestines) move downward. Severe prolapse is when these organs come out externally, where a bulge can be seen or felt. Mild or moderate prolapse is more common. Symptomatically, prolapse can feel like pressure, heaviness or aching in the pelvic floor, or the feeling of a tampon falling out. Prevalence of prolapse has been difficult to confirm, especially given the fact that only 4-10% of women who have prolapse report symptoms. One research study discovered prolapse in 32% of women and a different study found prolapse in 98%, and other studies have shown numbers in between. While we are not sure exactly how many women it affects, it is a large percentage of middle-aged and older women. Risk factors for prolapse include increasing age, obesity, chronic constipation, vaginal delivery especially with trauma or episiotomy, smoking and giving birth to large babies. Women who have had a c-section are less likely to develop cystocele and rectocele but still are likely to develop uterine prolapse. Terms such as cystocele refer to which organ is prolapsed, in this case the bladder (see the picture for more details). There are different types of prolapse and you can have more than one at the same time. Prolapse is diagnosed with a pelvic exam (so ask your healthcare provider about it when you go next time) so you can know your body. The word prolapse can sound scary. And the statistics make you realize how many of us likely have some degree of mild prolapse without any symptoms. Don’t be afraid. I like to think of it as the organs have shifted during pregnancy, they were stretched and pushed down by baby. After delivery, our body is healing and reorganizing for up to a year postpartum. If you have prolapse right after having a baby, know that it will likely improve as you heal. If you have never had a baby or had a baby a long time ago, there is still hope. This is a wake up call to be proactive. We have control over our pelvic floor strength, and how we use our body all day long. What contributes to prolapse? Excess pressure, specifically downward pressure on the pelvic floor. Things like straining to have a bowel movement, pushing a baby out for hours. But also bearing down on your pelvic floor when you are doing strenuous activities such as lifting your kids, working out, even yelling. It is my belief that years of this excess pressure in combination with gravity and more hormone changes during peri-menopause may contribute to pelvic floor issues (such as prolapse and incontinence) later in life. While there are no studies to prove or disprove this, I believe that it is worth taking the time to work on your core and pelvic floor to help now and hopefully in the future. To be proactive, it is important to learn intra-abdominal pressure management strategies. Big words, right? What that means is learning how to use the inner core system functionally. The pelvic floor, abdominal wall, diaphragm, and deep back muscles all working together without putting excessive pressure on the abdominal wall or pelvic floor. A functional core system will not only help prolapse, but can also help with back pain and other issues as well. Unfortunately, it is not as easy as just doing one or two exercises. It is truly understanding where these deep muscles are and how to apply these concepts into your daily activities as well as other types of exercise. The goal is a functional, reflexive core system that provides support and stability. Whether you have prolapse or not, whether you have symptoms or not, right now is the best time to start. Permission to use copyright images from Pelvic Guru LLC. Experts estimate that 80% of Americans will experience low back pain during their lifetime. In the last three months, 25% of Americans have had low back pain. Low back pain can have many causes but the most common causes are musculoskeletal. Good news is that means conservative treatments often work! I am also a believer that a good rehabilitation program will not only help your back pain now, but help you avoid future back pain as well. No, you do not have to live with a “bad back” forever. Here are a few other things I wish everyone would know.
You are not your MRI. I have had many patients that come to PT who have had an MRI or other imaging. Sometimes the MRI is from 10 years ago, sometimes it is recent. Either way, I still perform a full evaluation which includes movement testing, flexibility, muscle and core strength, joint mobility, and more. It also includes looking at the pelvis, hip, lumbar spine, and any other surrounding structures that may be contributing to pain. An MRI does not show stiffness, weakness, or how someone moves. Just because imaging shows something is “wrong”, it does not mean that is the source of pain. A research study took imaging of people without back pain. They found disc bulges in 30% of 20 year olds, 60% of 50 year olds, and 84% of 80 year olds. This means that you can have a disc bulge with NO pain. Yes, disc issues can cause pain, especially initially but our bodies can heal. More research has found spontaneous regression (where the disc shrinks/heals) in 96% of disc sequestration, 70% of extrusion, 41% of protrusion, and 13% of bulges. This means that the further out the disc is protruding, the better chance it has of healing on its own. Pretty amazing, right? Our bodies are designed to heal. Imaging may be important if there was a traumatic injury (like falling off a ladder), or if there are signs of significant neurological involvements (such as leg weakness, coordination loss or bowel/bladder changes like sudden incontinence/loss of control). But other than that, save your time and money, and start with Physical Therapy. Keep Moving. When low back pain starts, a common response is to try to protect yourself. For many people, this leads to not moving that area or trying to lay down and rest more. Unfortunately, this can lead to stiffness and muscle weakness. It is important to keep moving. Avoid certain movements that cause pain, but usually that does mean you need to avoid everything. Look at the big picture. I often joke with my patients that I am treating the “leftovers”, especially when they are coming to Physical Therapy after dealing with low back pain for months or years. When we are in pain, our bodies compensate. Muscles often tighten up to protect us but this can also lead to muscle weakness and imbalances or different movement patterns such as limping or not putting as much weight on one leg. Unfortunately, when the pain subsides our bodies do not automatically reset. We need to consciously strengthen and retrain our bodies, which is possible but may need some guidance. Research has also shown an association between chronic back pain and pelvic floor dysfunction in women. 90% of women with chronic low back pain had pelvic floor dysfunction, with 80% of them having incontinence (leaking urine). So ladies, if you are leaking urine (yes, even a little bit), having pelvic pain or pressure, or pain with intercourse- you should seek help. Not only can it help resolve your issue but it may help with back pain, hip pain or another issue. Also keep in mind that stress levels, nutrition, and sleep can all contribute to our ability to heal. When our sympathetic nervous system is in charge, our body is in “fight or flight” mode and more easily overreacts to stimuli. This can cause more pain and impairs healing. We want our parasympathetic nervous system to kick in which is “rest and restore” mode. Deep breathing and meditation exercises are helpful to start calming down the nervous system and facilitating the healing process. If you want more guidance, get our free guide, 7 tips to help your Back Pain. And if you or a loved one is suffering from back pain, schedule a free virtual discovery session with an expert Physical Therapist to determine if PT is the next best step for you. And the best time to take action is now! By Dr. Rachel Miller, Physical Therapist, certified Pilates and group fitness instructor
There is so much to think about during pregnancy- your body, the baby, and figuring out everything you need for the baby. But the saying “you don’t know what you don’t know” is so true. I was an orthopedic Physical Therapist when I had my babies. But the lack of postpartum care and pre/postnatal education changed my path so I continued my journey and also became a women’s health/pelvic floor Physical Therapy. There is so much I wish I knew when I was pregnant, so I made this Top 5 list for you. 1. Exercise is beneficial As long as you have your birth provider’s permission, exercise is beneficial during pregnancy. Regular exercise can decrease the risk of gestational diabetes, decrease common discomforts, relieve stress, and build endurance. The American College of Obstetrics and Gynecology recommends 30 minutes or more of moderate exercise per day on most days of the week. Know that you may need to modify the intensity or type of exercise, especially later in your pregnancy. Avoid overheating, overstretching, and be careful with your balance as pregnancy progresses. Listen to your body and your birth provider. 2. You can be proactive While we cannot control everything that happens during pregnancy, we do have control over our posture, muscle activation, and how we perform everyday activities and exercise. As the baby grows, there will be increased pressure on the abdominal wall and pelvic floor which can contribute to diastasis recti and incontinence. What we can control is not putting even more pressure on the system. We can make sure our deep inner core system is functioning optimally. Learning these concepts during pregnancy can also assist with delivery and postpartum recovery. 3. You can (and should) prepare for delivery If you are planning for a vaginal delivery, there is a lot to learn. Everything from perineal massage to labor positions, comfort measures, and effective pushing techniques. I highly recommend taking a comprehensive birth class so you are prepared- mentally and physically for the amazing task that lies ahead. If you are planning for a c-section, make sure you know what that entails and your options for that day. 4. Learn about postpartum recovery BEFORE you deliver Trust me, once you are holding that baby you tend to forget about everything else (including your own body). The best time to learn about postpartum recovery is the last trimester of your pregnancy. Knowing how to reconnect with your deep core muscles, what to do/not do when taking care of baby, and what to check for (and ask your provider about) at 6 weeks postpartum is so important. Also knowing how to get back into exercise in a safe, smart way once you are ready. Learn about common issues such as diastasis recti, pelvic pain, incontinence, and prolapse. 5. Find your dream team There is nothing wrong with asking for help- during pregnancy, birth or postpartum. I wish I knew about doulas when I had my kids. There are birth doulas that can support you during birth, and postpartum doulas that help with the baby when you get home (even overnight). Also lactation consultants, mental health providers that specialize in pre/postnatal conditions such as anxiety and depression, and pelvic floor Physical Therapists that can help with pain, core weakness/diastasis recti, leaking urine/feces, prolapse and more during or after pregnancy. I highly recommend researching providers during pregnancy and making your dream team so you know who to call if you need. Having family and friends help with childcare and meals can help a lot. And don’t forget to make time for yourself. You deserve some self care time- whether that is a pedicure, a walk without the baby, or going to an appointment to help you recover, you are allowed to take care of yourself too. Remember your body is meant to do this. I find that many women prefer not to think about birth and postpartum when pregnant. They rather not know. I understand. But in hindsight, I wish I would have known what I do now. Understanding better labor and delivery positions and more effective pushing techniques, I truly believe my first birth would have gone differently. I think I would have not pushed so long, would have not torn as severely, would have avoided a vacuum assisted delivery, and that my postpartum recovery would have been much easier. You need to know what to expect, and what to ask for and how to advocate for yourself. Your body will thank you, now and in the future. If you want to learn exactly what you need to know about the above topics and so much more I have created an online self paced Proactive Pregnancy program or come in for a Pregnancy Prep session. It contains all of the information to guide you through pregnancy and postpartum. Please share this post with anyone you know who is expecting! |
Get your free guideJust click on the picture: 7 Tips to help your back pain feel better without pain medication, injections, or surgery or Post-baby Body Basics: what every Woman needs to know about their postpartum body. CategoriesArchives
September 2022
|
|
1113 S. Milwaukee Ave
Suite 203 Libertyville, IL 60048 |
Copyright ©2020. The Pilates PT LLC. All rights reserved

 RSS Feed
RSS Feed
